Before the coronavirus hit, the urgent care center where Glenn Hoffman ’77 works was seeing upwards of 100 patients a day. Today he and the staff treat fewer than 50 people daily and all of them present in one way or another with symptoms of COVID-19.
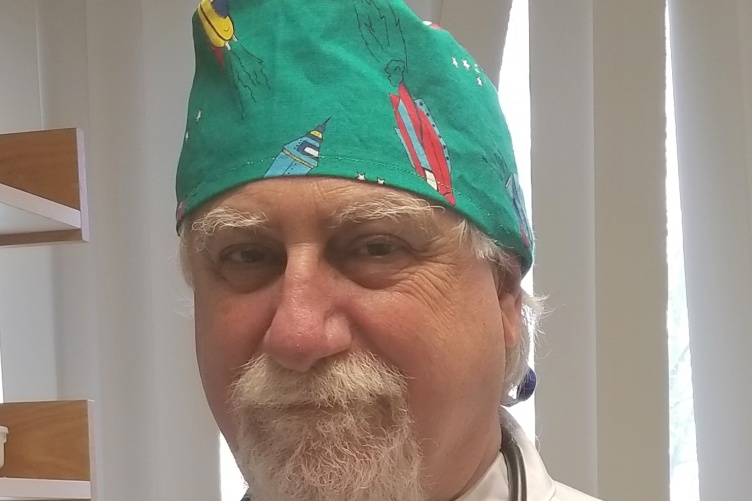
Hoffman is a physician assistant (PA) at Atrius Health in Braintree, Massachusetts. He is part of a team that includes a doctor, two nurses and three medical assistants. Toward the end of March, the healthcare center made the decision to treat only those patients who were suspected of having the coronavirus.
“Prior to COVID-19, we ran a very busy unit seeing upwards of 100 patients in a 12-hour day. When the virus hit approximately seven weeks ago, Atrius Health made the decision to make our site a purely respiratory unit for evaluating patients for COVID-19,” Hoffman says. “So, we are seeing 30 to 40 patients a day instead of our usual caseload because these evaluations can be time consuming.”
Patients with traditional urgent care complaints are seen at separate Atrius Health location — considered a "clean site” — so otherwise healthy people won’t be exposed to anyone who might have the virus.
"I’m in pretty good health and offered to continue my work. I have been a PA for forty years and this is what I am trained to do."
“We’ve diagnosed many cases of COVID-19; we have seen people, young and old, with a variety of symptoms from a little congestion to severe cough and shortness of breath. In the older population we are seeing low oxygen levels. These folks have a tendency to decline rapidly and are sent to the hospital,” Hoffman says.
The first month was challenging, he says, because there were limited test kits and stringent protocols for who could receive the tests: people in healthcare at risk of exposure, older people with preexisting conditions such as diabetes or heart and lung diseases.
“We felt like we were working with one hand tied behind our back,” Hoffman says. “This has improved, but it’s not perfect.”
Thankfully, he adds, the urgent care center has been well equipped with personal protection equipment from the start. The hardest part, he says, has been the mental fatigue; not knowing if the virus will hit again in the fall or winter.
Hoffman is 66. When Atrius Health made the change to treat patients with coronavirus symptoms, he was offered the chance to furlough but turned it down.
“Two other physicians that worked in our unit had significant health conditions and have left. I’m in pretty good health and offered to continue my work. I have been a PA for forty years and this is what I am trained to do,” Hoffman says.
He doesn’t just mean evaluate patients in these trying times: Hoffman has had training for Ebola and SARS.
At UNH, he was a health studies major in occupational therapy. During his senior year, he did a paper on alternative medical practice and read about physician assistants, something he had never heard of before. At the time, he lived in Newmarket, New Hampshire, and met a man who ran the small three-room health clinic on Main Street. Michael Lewis was a PA.
“He took me under his wing and showed me how to draw blood and suture. He taught me a great deal (about being a PA). I was sold on the idea and went back to school the year after graduation,” Hoffman says.
Prior to joining Atrius Health four years ago, he worked in the emergency room at Beth Israel Deaconess in Plymouth, Massachusetts.
“This clearly has been the most challenging part of my career,” Hoffman says. “I am getting close to retirement, but I feel I still have something to offer.”
-
Written By:
Jody Record ’95 | Communications and Public Affairs | jody.record@unh.edu