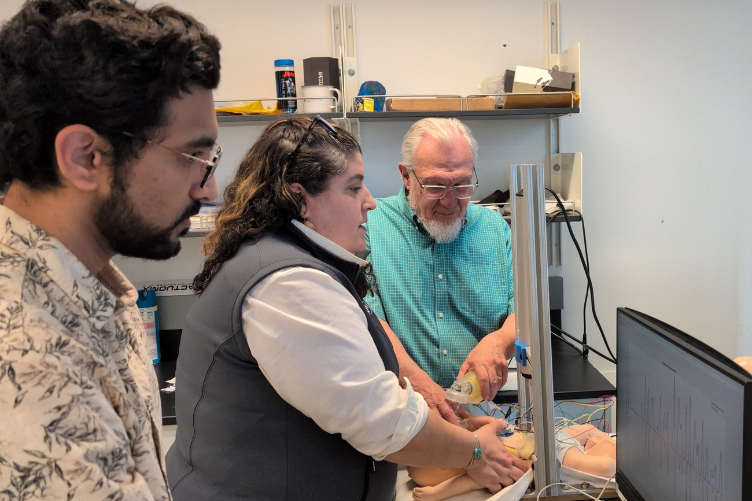
Prashant Purohit monitors data on the computer screen as Alyssa O’Brien, associate professor of nursing, and John LaCourse, electrical and computer engineering professor, practice CPR on a training mannequin that Purohit developed.
Driven by his passion for engineering and making a difference at home, Prashant Purohit is focused on helping practitioners improve the quality of cardiopulmonary resuscitation (CPR) they deliver to newborns.
Through his research project “Impact of Fatigue Levels and Bed Heights on Chest Compression Dynamics during Neonatal Cardiopulmonary Resuscitation: Real-Time Analysis,” Purohit built a mannequin training device and found that real-time visual feedback improves technique and reduces fatigue, boosting chest compression quality and practitioner efficiency during neonatal CPR.
Originally from India, Purohit earned his master’s in electrical and computer engineering at UNH and is now pursuing a Ph.D. His research was motivated by high neonatal mortality rates in developing countries such as India, Pakistan, Bangladesh and many African nations, where hospitals often can’t afford advanced CPR training mannequins that cost between $35,000 and $50,000.
“In a country like India, which is still developing and has such a large population, there are so many hospitals, but it’s difficult to get these expensive training devices into each one,” Purohit says. “That really concerned me. I started thinking: How can I create something more affordable? I realized the goal isn’t to simulate real-life emergency scenarios perfectly but to focus on training healthcare providers effectively.”
Interdisciplinary Partnership Fuels Research Project

Purohit’s research brought together expertise from engineering and healthcare. He worked closely with John LaCourse, an electrical and computer engineering professor and department chairman, and Alyssa O’Brien, an associate professor of nursing and a former labor and delivery nurse.
“CPR in adults has been fairly standardized for the past 25 years, with a focus on chest compressions and defibrillation,” O’Brien says. “But with newborns, it’s more complex because it usually involves both respiratory and cardiac issues.”
She adds that mechanical devices now assist with adult CPR, reducing fatigue during prolonged efforts, but such tools aren’t viable for newborns because of their wide variation in size, from preterm babies under five pounds to full-term infants over 10 pounds.
The nursing program provided Purohit with an old mannequin no longer in use, and he modified it with custom sensors, circuitry and code to measure the force applied to the chest, compression depth, chest recoil, CPR rate and rhythm practitioner fatigue levels.
“Whenever my students want to work in the medical field, I tell them, 'Go talk to the people who do this work daily,'” says LaCourse. “You can’t design effective tools in isolation. Nurses are the domain experts — they understand the real challenges, like how bed height affects fatigue or how arm strain sets in. That practical insight is essential if you want to build something that truly works in the field.”
Data That Could Improve CPR Training
To collect data, Purohit worked with 15 nursing professionals. Each participant performed chest compressions on the mannequin for up to 10 minutes using three different techniques—two-thumb, two-finger, and cross-four-finger — at varying bed heights simulated through an adjustable desk.
Using data and machine learning, Purohit developed a model to predict when fatigue will impact performance. Practitioners worked in pairs — one performing compressions, the other providing ventilation — and they would switch roles when the person performing compressions reached a predicted fatigue level.
Purohit found that even trained professionals weren’t always aware when fatigue or technique breakdowns were affecting performance:
- Many experienced practitioners performed compressions too quickly — 140–150 per minute instead of the 120 recommended by the American Heart Association (AHA).
- Faster compressions limit proper chest recoil (the return of the chest to its normal position after compression), crucial for adequate blood flow. Purohit's measurements showed the two-finger method achieved 93% recoil, the two-thumb achieved 84%, and the four-finger achieved 79%.
- Most practitioners began to lose form after just 40–60 seconds — well before the two-minute switch guideline by the AHA.
- Arm position and bed height significantly influenced fatigue and performance, with neutral bed height (elbows at 90 degrees) producing better outcomes.
- The two-thumb method at neutral height proved the most consistent, offering the best balance of depth, force, rhythm and fatigue resistance.
“The feedback from the experts was really positive,” Purohit says. “They were able to see how they were performing in real-time and adjust their techniques.”
Purohit noted the challenging dynamics involved in CPR — rhythm, recoil, depth, force — and how difficult it is to get them all right at the same time. He says the collaboration with O’Brien and the nursing program was essential for him setting up a realistic study and knowing what to measure, while O’Brien credited Purohit’s engineering skills for building a reliable device that gives practitioners real-time feedback.
“You don’t always realize when you’re getting tired or even hurting yourself during a real-life emergency,” O’Brien says. “Your adrenaline is going, you’re focused on saving the baby, and you may not notice your technique is slipping. But when we watched the real-time data, we could see the moment our performance changed before we even felt it. That kind of feedback is not just helpful for the patient; it helps protect the nurse, too.”
 Turning Innovation into Impact
Turning Innovation into Impact
Purohit has presented his research at multiple venues, including a national nursing conference in Philadelphia, university symposiums and other academic events. The response has been positive.
As he looks to the future, Purohit hopes to enter the medical device industry and to focus on developing an affordable mannequin to help practitioners in under-resourced areas train in neonatal care. He’d like to add audio feedback that provides real-time verbal coaching during compressions, telling practitioners when to "push harder" or "allow full recoil."
Another one of his goals is to develop a “smart cloth” with embedded sensors that could be placed over inexpensive mannequins and connected to a mobile app, offering accessible CPR training solutions.
“Every time we talked with the experts, something new came up, a new idea for the next component. That's the exciting part of research. Every day is a new day and a new challenge,” Purohit says.
Prashant Purohit discusses his research project
-
Written By:
Aaron Sanborn | UNH Paul College & CHHS | aaron.sanborn@unh.edu