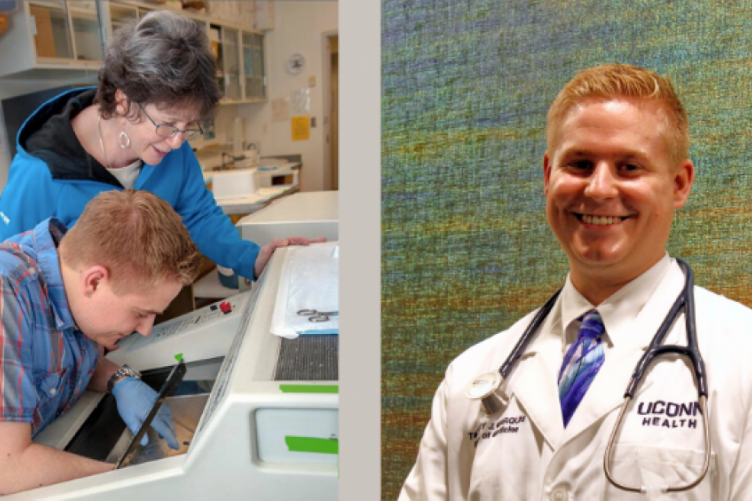
Tim Marquis , '15, and Dr. Stacia Sower.
Tim Marquis graduated with his bachelor’s degree in biomedical science from the UNH College of Life Sciences and Agriculture in 2015, and will complete medical school at the University of Connecticut this May. While he was an undergraduate, he conducted research at the New Hampshire Agricultural Experiment Station with Dr. Stacia Sower, professor emerita of molecular, cellular, and biomedical sciences, discovering a novel pituitary cell type in the lamprey. He credits his work with her and her mentorship with providing him the personal and professional qualities necessary for him to perform high-quality research in a world-class environment. As he fininishes medical school during the COVID-19 pandemic and prepares to start his residency at Yale, we asked him what the last few months have been like. Here is what he told us.
May 11, 2020, I will officially be Timothy Marquis, MD. As I approach this major milestone and reflect on my last four years in medical school at UCONN School of Medicine (UCONN SOM), I cannot help but feel a mix of conflicting emotions. I am incredibly proud and excited to become a doctor – a dream I have had since I was 13. Yet, I am also remarkably disappointed, as well as apprehensive about the next chapter in my journey.
COVID-19 Overtaking Normalcy
The past several months have been a whirlwind with COVID-19 overtaking the normalcy of all of our lives. As fourth-year medical students, my peers and I were in the midst of completing our required clinical rotations; anxiously awaiting the results of the 2020 Match, on Friday, March 20 at noon, to learn where we would each be trained for residency; and completing the necessary paperwork and requirements to graduate in May.

from the UNH College of Life Sciences and Agriculture in 2015
At the beginning of Match week, we learned that the Match day ceremony would be cancelled, as many schools were also doing across the country. While we were unable to open the traditional envelope with our Match results at noon, I was fortunate to be surrounded by family as I “opened” an email instead. I was absolutely thrilled to learn that I matched at Yale School of Medicine for Primary Care Internal Medicine Residency.
However, only days later, we learned that our graduation was cancelled. As a member of the first class of a new medical curriculum at UCONN SOM, we were pioneers – experiencing both the highs and the lows that come with experimenting with a radically different teaching pedagogy for the first time. Yet, we had successfully navigated the new curriculum, and were approaching our long-awaited destination of graduation. Thus, it goes without saying how meaningful our graduation was for all of us. Over the past several weeks, details have slowly trickled in that we will, in fact, have a graduation, but it will be a virtual ceremony. Although it is not the same as the in-person “Pomp and Circumstance,” it is nice to still be honored in some way.
Caring for Patients
One of the special aspects of the medical school curriculum, which is unique to UCONN SOM, is the opportunity to begin caring for patients in a longitudinal, weekly, continuity primary care clinic throughout the first three years of school. I chose to continue this during fourth year. It has been an amazing experience, being able to step into the role of a resident, caring for my own panel of patients with a high degree of autonomy, under the mentorship of a clinical preceptor, Dr. Rabitaille, who I have worked with for the past three years.
However, my clinic experience was cut short, like all other clinical rotations and courses, we were barred from attending for the remainder of the academic year, due to COVID-19. While I had begun the process of saying goodbye to my patients back in January and February, there are many patients that I never had the chance to see one last time. It has been deeply unsettling not to have that closure.
It is one of the reasons why I chose a primary care internal medicine program over a traditional categorical internal medicine program for residency – to spend more time caring for patients over the course of years, in the outpatient primary care setting, rather than predominantly in the inpatient wards, which are like revolving doors. It is also one of many reasons why I aspire to become an oncologist. I enjoy the privilege of caring for people over the long-term and of being able to form meaningful, lasting relationships with them as their healthcare provider.
Preparing for Yale and the Future
Over this three-month transition period suspended in limbo, I have remained extremely busy. While many of my classmates are wrapping up their remaining required clinical rotations virtually, somehow, I fortuitously managed to plan my fourth year perfectly – completing all of my required rotations early – so I am done, just waiting patiently to graduate. But unlike many medical students transitioning to residency, I am not selling all of my belongings and moving into a new rental home.
Instead, my fiancé, a fellow Wildcat, and I, whom I got engaged to on Christmas Day 2019, are in the process of buying our first home close to Yale. Consequently, I have been inundated with the moving parts of the closing process, as well as lots of packing.
At the same time, I have been working on completing and submitting several research papers. In particular, I have been working endlessly on a first-authored manuscript called, “Transforming Medical Education Through Student-Led Educational Quality Improvement (sEQI),” which is the culmination of my research during medical school.
I had the unique opportunity, as one of three of my classmates, to comprehensively and critically review and revise our new medical curriculum at UCONN SOM, through a novel student-led quality improvement process that delved into both general and specific aspects of the curriculum, including rewriting course syllabi, objectives, and exam questions, as well as recommending new learning materials – our objective being to improve student satisfaction in the learning process and environment.
Subsequently, as a result of our quality improvement research project, student satisfaction increased on average 12 percent and increased by as much as 43 percent, from the year prior. Some classes even attained 100 percent student satisfaction. In contrast, after faculty-only reform, student satisfaction decreased on average 7 percent and decreased as much as 28 percent, from the year prior. It was a tremendous honor to be a part of this project.
Importance of UNH Research Experience
I directly attribute my research at UCONN SOM to my research experience with Dr. Stacia Sower while an undergraduate at UNH. Dr. Sower is, without a doubt, the best role model in academia and research whom I have ever had the privilege to work. She helped me hone the personal and professional qualities necessary to perform high-quality research in a world-class environment. I have never met a more dedicated educator and researcher.
While my research focus pivoted dramatically from bench research in the basic sciences to medical education, the same qualities and skills are integral. For example, there is a phrase Dr. Sower always said, that I remember and carry with me to this day, “It takes as long to write the paper as it does to do the research." Additionally, Dr. Sower would never let a manuscript draft sit on her desk for more than one week before responding thoroughly – usually, she would get back to me the same or next day.
The perseverance, dedication, and attention to detail that I learned from Dr. Sower, are traits that I strive to incorporate every day while caring for my patients. Notably, at every single residency interview I attended, my interviewers were remarkably interested in the research I had done, not only at UCONN, but also at UNH with Dr. Sower. The residency program director at Yale was particularly curious about my lamprey research, as he was a marine biology major as an undergrad!
Anxiety about the Future
I would be lying if I said I wasn’t worried about getting sick with COVID-19 during residency. Our radiology professor recently gave a presentation on COVID-19, and he presented a case of a previously healthy, young healthcare professional in their mid-thirties, with no underlying medical conditions, who ended up almost dying from the sequelae of COVID-19 despite receiving the highest level of care in the intensive care unit.
UCONN students are not allowed to participate in the direct care of patients who are positive, or being ruled out, for the virus. There are many different ways that students can help. For example, some are volunteering as babysitters for children of UCONN healthcare professionals.
One of the first things I learned 13 years ago during my training to become a ski patroller, was “scene safety.” You do not enter a medical scene if it isn’t safe for you as the provider, for you not only put your own life at risk, but you also burden the healthcare system by increasing the number of potential patients to care for. Healthcare providers go above and beyond the call of duty when caring for their patients, and often put themselves in vulnerable and unsafe situations that expose them to illnesses and harm, particularly if they have an underlying medical conditions that predisposes them to getting sick in the first place.
At UCONN’s John Dempsey Hospital, there are currently over half as many cumulative cases of healthcare providers sick with COVID-19 as there are cumulative patient cases. With such limited resources of personal protective equipment (PPE) across the United States, my ski patrol training really strikes home, and highlights the importance of balancing the care for others with your own care and wellbeing – a sentiment echoed by my residency program. Right now, PPE needs to be reserved for healthcare providers directly caring for hospitalized patients. Consequently, everyone needs to be careful about volunteering or other activities they are currently engaging in without having appropriate PPE. The decision to act now may subsequently preclude matriculating medical students from being able to begin caring for patients at the start of residency if they become ill with COVID-19 themselves. Therefore, it is important to recognize that sometimes waiting for the appropriate time to “help” is the most helpful thing we can do as medical students for our future patients and the greater public health of the nation.
It is with tremendous excitement, balanced with a moderation of anxiety, that I embark on residency during this unprecedented time. During this time of uncertainty, one thing I am certain of is that I am proud to be a UNH Wildcat, UCONN Husky, and rising Yale Bulldog!
-
Written By:
Lori Wright, '06G | NH Agricultural Experiment Station | lori.wright@unh.edu | 16038621452