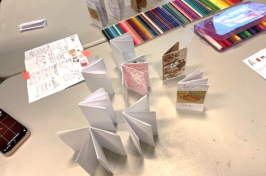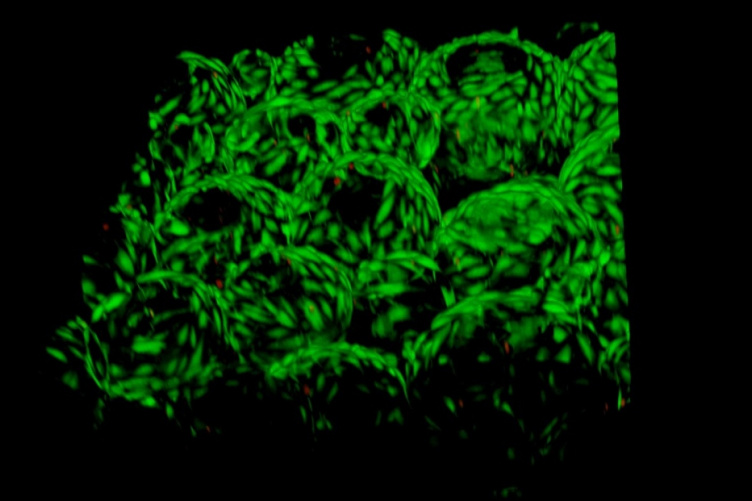
This 3D confocal microscope image shows human skin cells growing around and within the porous hydrogel. Credit: University Instrumentation Center at UNH.

UNH researchers have created an easy-to-make, low-cost injectable hydrogel that could help wounds heal faster, especially for patients with compromised health issues.
Wound healing can be complex and challenging, especially when a patient has other health obstacles that seriously impede the process. Often injectable hydrogels are applied to irregular shaped wounds, like diabetic ulcers, to help form a temporary matrix, or structure, to keep the wound stable while cells rejuvenate. The caveat is that current hydrogels are not porous enough and do not allow neighboring cells to pass through toward the wound to help it mend.
“While valuable for helping patients, current hydrogels have limited clinical efficacy,” said Kyung Jae Jeong, assistant professor of chemical engineering at UNH. “We discovered a simple solution to make the hydrogels more porous and therefore help to speed up the healing.”
“We discovered a simple solution to make the hydrogels more porous and therefore help to speed up the healing.”
In a study recently published in the journal of ACS Applied Bio Materials, the researchers outline how they made a macroporous hydrogel by combining readily available gelatin microgels — hydrogels that are a few hundred microns in diameter — with an inexpensive enzyme called microbial transglutaminase (mTG). Gelatin was used because it is a natural protein derived from collagen, a protein found in connective tissue in the body such as skin. Assembling these tiny microgels with mTG helped create a hydrogel with large-enough pores for the neighboring cells to move into the wound for repair. In addition, this new injectable formulation allows for the slow release of protein drugs to aid wound healing, such as platelet-derived growth factor (PDGF). The researchers compared conventional nonporous hydrogels with the new macroporous hydrogels, and found a notable increase in the migration of tissue cells inside the hydrogel, which is the hallmark of wound healing.
Along with diabetic ulcers, the macroporous hydrogel could help with other forms of healing on the skin, cornea, internal organs during surgery and even has military implications.
Jeong’s co-authors on the study are UNH graduate students Shujie Hou and Seth Edwards, undergraduates Rachel Lake ’19 and Chante Jones ’20 and postdoctoral researcher Shiwha Park.
This work was supported in part by the NIH COBRE Center of Integrated Biomedical and Bioengineering Research through an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences.
-
Written By:
Robbin Ray ’82 | UNH Marketing | robbin.ray@unh.edu | 603-862-4864