UNH research indicates that gut microbes play a significant role in the variable individual responses to pain management using opioids.
Despite their wide use and effectiveness, opioid pain medications can lead to addiction in some people. New Hampshire has had among the highest drug overdose death rates in the nation within the past decade. At the University of New Hampshire (UNH), Cheryl Whistler is investigating why opioid response and addiction susceptibility differs between individuals and whether unseen but essential partners in our health and function — microbes in our guts — play a role. The answer could help in developing healthcare strategies to reduce opioid addiction risks.
“Patients who need pain relief, such as after surgery, often find that a prescribed opiate no longer works as well over time, and more is needed to have the same effectiveness,” says Whistler. “We demonstrate that administering butyrate, a simple intervention that can be added to the diet, could prevent analgesic tolerance to opioids, which is an early step to opioid addiction.”
Whistler, a professor in the department of Molecular, Cellular, and Biomedical Sciences in the College of Life Sciences and Agriculture, worked with a research team that included her sister Jennifer Whistler, a professor at the University of California-Davis, and Izabella Sall, who earned her doctorate from UNH in May 2025. They found that butyrate, a molecule produced by microbes, may contribute to the variable responses and to the maintenance of opioid effectiveness in some people. Their findings, published in Gut Microbes, point to a possible strategy to help maintain opioids’ painkilling properties.
Opioids and gut microbiota
Genetic differences between humans can help to explain different responses to drugs, but even mice bred to be as genetically identical as possible show variability in opioid response. Over time, most mice and humans develop opioid tolerance — a condition that reduces the drug’s ability to block pain. Taking higher doses can lead to increased dependence and opioid use disorders, with a high risk of overdose. Understanding why people respond differently to opioid medications provides the opportunity to tailor their administration to maximize clinical effectiveness and minimize serious side effects.
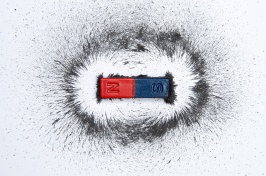
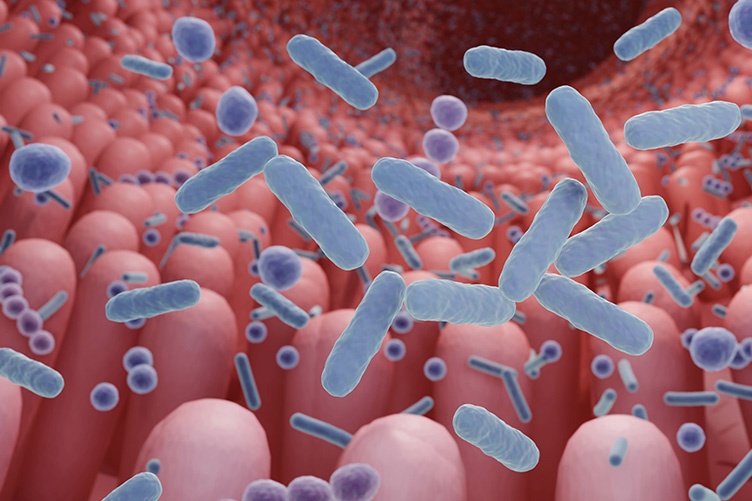
Whistler focuses on gut microbiota, an important player in a wide range of functions. Gut microbes produce molecules that affect the brain, such as neurotransmitters, and microbial populations can differ between individual people. The ways in which they influence health and disease are the subject of many ongoing studies.
Regardless of the individual, there is an array of microbial species and communities, collectively known as the microbiome, present in everyone’s gut. Some are actively beneficial, such as Lactobacillus, which has been found to help suppress inflammatory responses. Others, such as Streptococcus, can be pathogenic in certain contexts. While there is no “ideal” gut microbiome, maintaining a balance between the various microbial communities is thought to contribute to healthy function.
"Butyrate, whether produced by microbes or added to the diet, may provide protection from opioid tolerance"
It is well recognized that opioids disrupt gut microbe balance. Prior research has also suggested that the disruption may contribute to increased tolerance to opioids, lessening their painkilling effectiveness. Whistler and her research team delved deeper, fully characterizing the gut microbe populations in mice prior to opioid (morphine) ingestion and how morphine affected them over time.
The microbiota were highly variable even before morphine exposure, despite the mice being the same age, sex and genetic makeup. Importantly, the researchers found consistent, noteworthy differences between the microbiota in mice that developed opioid tolerance and those that did not.
Possible mechanisms for avoiding opioid tolerance
In just under 40% of mice, morphine retained full pain-blocking effectiveness. In the remaining 60%, the mice developed tolerance to morphine, a condition that would result in needing higher levels of morphine for effective pain management. For the animals in which the drug’s effectiveness waned, the researchers observed that microbiota instability developed more quickly, and their overall population of beneficial microbes were depleted earlier. What most distinguished the mice that did not develop morphine tolerance was the retention of microbes associated with the production of butyrate, a short-chain fatty acid.
Butyrate has several beneficial functions, serving as an anti-inflammatory and enhancing intestinal barrier integrity. While the most abundant microbe found to be associated with non-tolerance, Akkermansia muciniphila, does not produce butyrate itself, it fosters the growth of butyrate producers and stimulates mucin production. The researchers also found that dietary butyrate supplementation blocked opioid tolerance when compared with a control supplement.
“Our findings provide evidence that gut microbiota have important effects on opioid response and the development of tolerance,” says Whistler. “More research is needed to further explore the mechanisms involved, but butyrate, whether produced by microbes or added to the diet, may provide protection from opioid tolerance. If so, clinicians can apply these findings to use opioids more effectively for pain management, with lower associated risks.”
-
Written By:
Mark Wanner | College of Life Sciences and Agriculture | Mark.Wanner@unh.edu