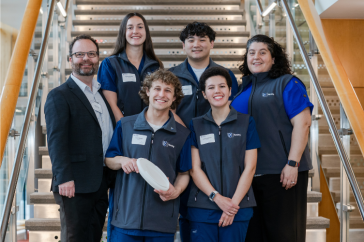
Will Lusenhop and Alexa Trolley-Hanson of CHHS
UNH has long contributed to the healthcare workforce in New Hampshire, and now a new grant is helping train professionals to work in behavioral health settings in underserved parts of the state.
The $1.9 million grant from the Health Resources and Services Administration (HRSA) will help put master’s-level social workers and occupational therapists to work in primary care settings that integrate behavioral healthcare. Part of the college’s Pathways to Behavioral Health Careers project, the grant will provide stipends to 116 social work and occupational therapy graduate students to support the costs of completing their fieldwork in behavioral health settings. Ultimately, the project will help put more professionals with this training into rural and medically underserved areas in New Hampshire, where they are most needed.
“Increasing the number of healthcare professionals who are trained to provide integrated behavioral healthcare is a priority for the college and the university," says Mike Ferrara, dean of the College of Health and Human Services.
During the first year of the grant the focus is on developing a comprehensive training program, including intensive clinical placements for master’s students in settings that provide primary care and build in behavioral healthcare as a core component of practice.
Will Lusenhop, clinical assistant professor in the department of social work, is director of the Pathways to Behavioral Health Careers project. The timing of it, he says, aligns well with other efforts happening in the state.
"We are finally breaking down the walls that have separated physical health, mental health and substance abuse and addiction problems as unrelated to each other,” he says. "These issues are inextricably linked, and the outcomes require us to take a holistic approach to care, including a focus on the social determinants of health, such as access to care, the role of poverty and environmental factors that influence our well-being."
Real-world experience
Master of social work student Emily Berman is completing her internship at Manchester Community Health Center (MCHC). Berman, who became interested in social work in high school when her father was diagnosed with pancreatic cancer, says she wants to be able to provide the kind of support to others that she received.

“I was helped by many social workers during that time, and I loved the idea of eventually being able to provide the same type of comfort and support that they gave me to other people who need it,” she says.
Berman admits being intimidated at first by the thought of working alongside medical practitioners at MCHC, but a tour of the center during her interview put her at ease.
“It was nice to see everyone — counselors, case managers, doctors and nurses — all working together to create the best possible outcomes for their patients,” she says.
And now, the hands-on experience is equipping her for a challenging and meaningful career on the front lines of healthcare.
“The integration of behavioral health into primary care is important for two main reasons: increased access and reduction of stigma,” Berman says. “Offering both services in one setting makes it so much easier for patients. It also normalizes mental and behavioral health treatment. So many people think that if you see a counselor, it means that something is 'wrong' with you, but that's not the case. Everyone feels stress; everyone goes through hard times, and having an unbiased person to talk to for guidance and support can be incredibly helpful.”
Her internship, she says, “is really giving me a variety of experiences and preparing me to be able to work in any type of setting.”
Occupational therapy’s role in behavioral health
The role of social workers in behavioral health settings — such as counseling and case management — is obvious, but what about occupational therapists? While they may be best known for providing therapeutic support to people with physical or cognitive challenges, occupational therapists provide a holistic approach to
“Occupational therapists often work as part of a medical team to provide services that are focused on helping people develop and maintain positive behavioral health."
assessing and supporting a person’s strengths, challenges, activities and environments.
"We help people achieve both mental and physical health through facilitating participation and engagement in occupations — the meaningful, necessary and familiar activities of everyday life,” says Alexa Trolley-Hanson, clinical assistant professor in the department of occupational therapy and a core faculty member on the HRSA grant.
"Occupational therapists often work as part of a medical team to provide services that are focused on helping people develop and maintain positive behavioral health, prevent behavioral health challenges and support people in their recovery," says Trolley-Hanson.
In the new and emerging models of integrated care, their participation is more important than ever. To that extent, Trolley-Hanson is overseeing development of a program of study that will lead to a certificate in primary care behavioral health.
Partnering across the state
Integrated behavioral health is an evidence-based, rapidly expanding area of practice throughout the country.
"This practice innovation seeks to redesign primary care such that physical, mental and behavioral problems are addressed early, often and are a regular component of our healthcare visits," says Lusenhop. "The goal is to catch problems early, improve the quality of the patient’s experience and lower costs by reducing the progression of chronic health conditions."
UNH's Behavioral Health Initiative: Working Better Together
To address the behavioral crisis in New Hampshire, including complex issues of mental health and substance abuse disorders, UNH has launched a Behavioral Health Initiative across its campuses.
Led by the College of Health and Human Services, the initiative aims to determine how UNH can better serve the behavioral health needs of the state. Working with UNH faculty, staff and students, the state, public and nonprofit sectors and the business community, the initiative will be developing strategic recommendations for aligning the academic curriculum with workforce needs, conducting solutions-oriented research on behavioral health to inform public policy and enhancing behavioral health initiatives within the UNH community.
In New Hampshire, UNH’s Institute for Health Policy and Practice, through its NH Citizens Health Initiative, has been working toward that goal for several years, along with many stakeholders throughout the state. The Behavioral Health Integration Learning Collaborative was formed in 2015 to examine how the state can best address the complex needs around behavioral health within the context of primary care. There are more than 60 members of the collaborative, and they represent primary care practices, health systems, behavioral health providers, healthcare payers and public citizens across New Hampshire.
Through its research, the collaborative has demonstrated that integrated behavioral health and primary care benefits residents throughout the state, increasing the quality of healthcare and lowering costs. The group is an integral partner in the effort to increase the behavioral health workforce in the state.
“The Pathways to Behavioral Health Careers project will help develop a much-needed workforce for integrated behavioral health,” says Jeanne Ryer, director of the NH Citizens Health Initiative. “It’s a great opportunity to help our UNH students get on-the-ground experience in integrated New Hampshire practice settings.”
-
Written By:
Callie Carr | UNH College of Health and Human Services | callie.carr@unh.edu | 603-862-0970