Gale Carey, professor of nutrition, and her team of researchers found that laboratory rats that were exposed to polybrominated diphenyl ethers, or PBDEs, experienced a disruption in their metabolism that resulted in the development of metabolic obesity and enlarged livers in rats.
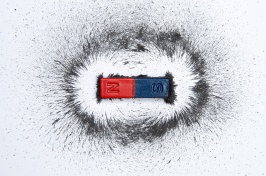
Chemicals used as synthetic flame retardants that are found in common household items such as couches, carpet padding, and electronics have been found to cause metabolic and liver problems that can lead to insulin resistance, which is a major cause of obesity, according to new research from the University of New Hampshire.
The research was conducted by Gale Carey, professor of nutrition, and is funded by the NH Agricultural Experiment Station at the UNH College of Life Sciences and Agriculture. Carey and her team of researchers found that laboratory rats that were exposed to polybrominated diphenyl ethers, or PBDEs, experienced a disruption in their metabolism that resulted in the development of metabolic obesity and enlarged livers.
The research results are presented in the current issue of the Journal of Toxicology and Environmental Health. In addition to Carey, the research team includes W. Kelley Thomas, professor of molecular, cellular, and biomedical sciences, and director of the UNH Hubbard Center for Genome Studies; Kylie Cowens, a recent graduate of UNH’s master’s program in nutritional sciences; and Stephen Simpson, a laboratory technician at the UNH Hubbard Center for Genome Studies.
In this research, fat cells isolated from rats dosed with high levels of flame retardants daily for one month developed a sensitivity to hormones that was similar to the sensitivity experienced by people who are overweight: the fat cells became more sensitive to epinephrine and less sensitive to insulin.
“One of the hallmarks of somebody who is becoming diabetic – and often this accompanies weight gain – is that their fat cells become sluggish in their response to insulin. With epinephrine, the fat cells more easily release the fatty acids into the blood stream and if those fatty acids are not used, they promote insulin resistance,” Carey said.
“Those two features – insulin resistance and epinephrine sensitivity – are two features of fat cells from people who are above normal weight. And that’s what we were seeing in our rats. Even though our rats had not gained weight, they were experiencing ‘metabolic obesity’,” she said.
The cause of the flame retardant-induced insulin resistance is unknown, but one possibility is the suppression of a key metabolic enzyme – phosphoenolpyruvate carboxykinase, or PEPCK – in the liver. PEPCK is responsible for sugar and fat metabolism. In their current work, Carey and colleagues confirmed earlier findings that the activity of PEPCK dropped by nearly 50 percent in livers of rats exposed to flame retardants for just one month, compared to controls. They went on to demonstrate that this drop in enzyme activity was reflected in similar drops of the amount of PEPCK protein as well as PEPCK message – the latter of which serves as a template to make the PEPCK protein. So the flame retardants appear to be interfering with PEPCK gene expression.
What does this mean physiologically? “Because PEPCK regulates production of the backbone of the fat molecule, if the backbone isn’t made, the fatty acids that usually attach to this backbone have nothing to attach to. Their levels can rise in the liver and the blood. And it is elevated fatty acids that can lead to insulin resistance,” Carey said.
The researchers found that the ability to create the backbone for the fat molecule was suppressed by 42 percent in liver tissue from rats treated with flame retardants compared to controls. Whether or not this decrease has health-associated relevance remains to be determined.
“Being obese or overweight increases one's risk of many diseases including Type 2 diabetes, high blood pressure, coronary heart disease, stroke, gall bladder disease, osteoarthritis, sleep apnea and certain cancers,” Carey said. In 2003, overweight and obesity-related medical expenses were 9.1 percent of total U.S. medical expenses at about $80 billion. New Hampshire's portion of this expense was $302 million.
“Despite the plethora of resources devoted to understanding the roles of diet and exercise in the obesity epidemic, this epidemic continues to escalate, suggesting that other environmental factors may be involved. At the biochemical level there is a growing body of experimental evidence suggesting certain environmental chemicals, or ‘obesogens’, could disrupt the body's metabolism and contribute to the obesity epidemic,” she said.
This material is based upon work that is supported by the National Institute of Food and Agriculture, U.S. Department of Agriculture, under award number 223362.
Founded in 1887, the NH Agricultural Experiment Station at theUNH College of Life Sciences and Agriculture is UNH’s original research center and an elemental component of New Hampshire's land-grant university heritage and mission. We steward federal and state funding to provide unbiased and objective research concerning diverse aspects of sustainable agriculture and foods, aquaculture, forest management, and related wildlife, natural resources and rural community topics. We maintain the Woodman and Kingman agronomy and horticultural farms, the Macfarlane Greenhouses, the Fairchild Dairy Teaching and Research Center, and the Organic Dairy Research Farm. Additional properties also provide forage, forests and woodlands in direct support to research, teaching, and outreach.
-
Written By:
Lori Tyler Gula, PhD | NH Agricultural Experiment Station | lori.gula@unh.edu | 603-862-1452