Photo courtesy Kendal Bush Photography
Alyssa O’Brien’s undergraduate experience is similar to many. When she enrolled at UNH in 1998, she had no idea what she wanted to do. So, she took classes in biology and social sciences, among others. After her freshman year, still frustrated that she didn’t have a definite path forward, her mother said to her “you’re taking a lot of classes that revolve around helping people. Have you thought about nursing?” At that point, her future was clear.
O’Brien, who was raised in Salem, New Hampshire, took an intro to nursing course and was hooked. Fast forward 20-plus years and she is now back in Durham, this time as an assistant professor of nursing, where she teaches courses on maternity, human development and public health nursing.
“It was like coming home,” she says of her return. After earning both her undergraduate and graduate nursing degrees at UNH, and working in the Family Center at Exeter Hospital for several years, she went to the University of California, San Francisco to pursue a Ph.D. in nursing.
O’Brien was recently recognized by the New Hampshire Nurses Association with an Excellence in Nursing award for her teaching and research.
Q: How would you describe your research?
Essentially my research focuses on the intersections of parental mental health and family stress and coping in early parenthood. I am specifically interested in how we teach practitioners and patients about parental mental health, how we assess families and develop family interventions around parental mental health to improve family outcomes.
Q: Why is this research important? In other words, why should people outside the scientific or academic community care?
I think that it is really easy to forget that often a stressful event or a diagnosis impacts an entire family and not just the patient experiencing it or receiving the information and coping with changes. When a parent is experiencing depression or anxiety, it is not only impacting their own health, but it is changing the family’s abilities to cope with all the demands placed upon them. They often need support and interventions that consider the whole family. But often, as care providers we are not trained to view the issue this way, rather we are taught to focus on the illness or diagnosis and the patient. You hear the term “patient centered care” a lot. In our nursing textbooks, in hospital and provider patient bills of rights, patient centered care is the primary focus. Looking at the family as a whole is often an afterthought, perhaps when the family has reached a crisis point. Family focused care improves patient and family outcomes, but it takes more time and is often harder to navigate. I want to make that easier for care providers.
Q: What are the most interesting findings from your research?
What I have found in multiple studies and quality improvement projects is that patients, students, educators, nurses, and primary care providers all believe that assessment, intervention, and education regarding parental mental health and support is valuable and important for successful family care. However over and over again I hear the response “I just feel like I don’t have the time. I know it is important, but when am I going to do it.” Whether that means to teach students or patients about it, or to assess children and their parents in primary care settings, using educational interventions, or making referrals for patients and their families, the health care system is just overwhelmed and people feel like they want to be doing these things, but they cannot. I want to find a way to make this easier and more consistent.
Q: What's your favorite course to teach and why?
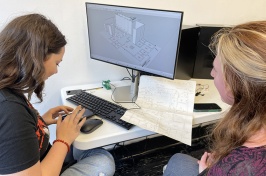
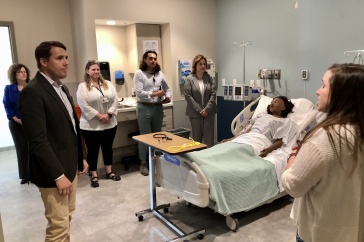
I am a family nurse to the core, having worked in adult health, maternity, pediatrics, the newborn nursery, and in community health. So my favorite course is Maternal Newborn nursing. The truth is, I am a storyteller. I find that students can relate to the course material or complex issues if they can associate it with a clinical situation, a case study, something that makes it real to them. However, many students have not experienced these issues in the clinical setting and it really helps for them to hear the story of a postpartum hemorrhage or a newborn resuscitation so they can remember key elements of care. I wrote a request my second year at UNH to get new maternal simulation equipment for our lab and the students have enjoyed using the simulator because it gives them another opportunity to “make it real” in their minds by responding in the moment. I am really looking forward to using the family nursing lab space at the new Health Care Simulation Center. There are a lot of patient care situations that students are not able to experience or maybe don’t have the time to process in the clinical setting and I know that in a simulation environment, their understanding of those emergency situations will become much deeper.
Q: So far in your career, what do you consider to be your greatest achievement?
As I am sure you can guess, for me it is all about the human connections; this is why I became a nurse in the first place and it has always felt like the right fit for me. I think that my research is very personally satisfying and mine is very relatable and deeply important. I love it when I am talking about my work and someone says “Oh, that same thing happened to me when my kids were little.” It always makes me smile, because as a parent, I have been there too. But I have to be honest, I think the moments in my career that stick out the most in my mind are those when I am working with students to successfully overcome a challenge, whether it be collaborating on their research, helping them improve their grades in courses in which they are struggling, talking them through career decisions, or even supporting them through personal crises and connecting them with campus resources. I find these human connections to be the most meaningful to me and I often hear back from them years into their careers to say thank you or to ask for advice about a professional decision. And although I didn’t need the NHNA award to make this meaningful to me, it certainly felt very affirming.
-
Written By:
Callie Carr | UNH College of Health and Human Services | callie.carr@unh.edu | 603-862-0970