Michele Loos will never forget the first patient who died on her watch. He was an elderly man who couldn't read or write. She was a 30-something UNH nursing student on her senior practicum. Had they met on the street, she would have assumed they had nothing in common. But as he lay dying in the Concord (N.H.) Hospice House, she became intimately involved in the routines of his daily life, shaving his face and feeding him through a tube. Because he had a tracheotomy, he couldn't speak. How, she wondered, could she possibly communicate with him?
So much, she discovered, could be conveyed through the eyes alone, and this man had huge dark brown eyes. He could also mouth words and point to yes or no on a whiteboard. There was a picture of him in military uniform on the dresser and his niece came to visit, but Loos got to know her patient over several months mainly through observation, seeing how he enjoyed the birds outside his window, how he laughed at gentle jokes in spite of his pain, and how he reveled in a cup of coffee twice a day, even if he could only manage a sip.
When it came time to leave for her winter break, Loos wept, convinced that the man would no longer be alive when she came back. But she returned to work a couple months later to find him still there, very near death. Her colleagues were convinced that he had waited for her, as the dying sometimes seem to do—hanging on, perhaps, until a certain person arrives or calls in from afar.
Over the break, she had received her nursing license and now, for the first time, she was in charge. She sat by his bedside, calming him in his agitation and delirium, reassuring his family and encouraging them to sit close to him. When it was over, she felt at peace. "I knew that we had completed something we had begun," she recalls. "He wasn't in pain, and this is what he wanted." Just as important was guiding his family through a night they would remember for the rest of their lives.
Loos likens the hospice nurse to "a midwife who can get you through this life to the next existence." It is a job she loves, and she has helped a number of patients and their families through this transition. But she has also acted as a midwife, on a much larger scale, to a new program at Wentworth Douglass Hospital in Dover, N.H., over the past year. It is no exaggeration to say that she has helped to transform the treatment of severely or terminally ill patients throughout the hospital. Most of her co-workers have no idea that she's been a licensed nurse for a mere three years.
Like most of the graduates of UNH's new direct-entry master's in nursing program, Loos came to nursing as a second career after years of working in another field. The program is designed to help ease the nursing shortage, which is projected to worsen as aging baby boomers simultaneously reduce the supply of, and increase the demand for, nurses. The goal is to produce highly educated nurses who can provide excellent bedside care, lead others in a clinical setting and teach future nurses. Research has linked the number—and education level—of nurses in a hospital to patient survival rates. For anyone who might need medical care in the upcoming years, the success or failure of efforts to address the nursing shortage could be quite literally a matter of life and death. As Loos demonstrates, good nursing can also enhance the quality of life, at any stage.
Not so long ago, points out Sue Fetzer, UNH associate professor of nursing and president of the New Hampshire Nurses Association, there were basically three career options for women: teaching, nursing and mothering. Now, she says, it's more like "What can women not do?" When Loos first attended UNH in the 1980s, business was a popular major for women. By the time she graduated in 1990 with a degree in business administration, however, she already knew that she wanted to be a nurse. She enjoyed working part time in a hospital, where, she discovered, she was unfazed by things like peeling socks off the feet of a homeless person. Nevertheless, she was paying for her own education, and going to school for another three years was out of the question. After graduation, she worked in a series of jobs in insurance and journalism.

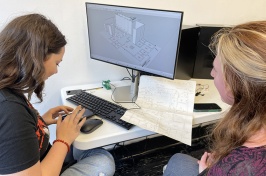
DYNAMIC DUO: Michele Loos '90, '06G and Dr. Patrick
Alix have transformed end-of-life care at Wentworth
Douglass Hospital in the last year.
In recent years, publicity about the nursing shortage and attendant increase in salaries has attracted people to nursing as a second or even third career. After Sept. 11, Loos thought, "What am I waiting for?" and began taking some courses toward her goal. When she took her anatomy and physiology exam, she was pregnant with her third child and so far along that she could barely fit between a classroom desk and attached chair. In 2003, she became a member of the first class in UNH's direct-entry master's program, one of about 50 such programs around the country that enable people with college degrees outside the field to become nurses—rapidly. Because there is a shortage of nursing educators, as well as nurses, demand for seats in these programs far exceeds supply. In 2005, the National League for Nurses reported, 147,000 qualified applicants were turned away from U.S. nursing-education programs at all levels. At UNH, which plans to expand its direct-entry program next year, 100 students from across the country and beyond applied for 24 spaces in 2006. Virtually all of the applicants were fully qualified, and eight of them had perfect 4.0 GPAs.
The direct-entry program is designed to be fast—not easy. On the first day of an eight-week course in pathophysiology, Loos recalls, it was more than a bit ironic to hear a professor of nursing announce, "If you have a fever of 104, stay home, but if you have diarrhea or you're throwing up, take whatever you have to take. Do Not Miss Class." Going to school year round, the students spend the first year and a half preparing for the national licensure exam; the remaining half year is spent doing graduate work and research. At the same time, they devote 16 to 32 hours a week to clinical rotations in hospitals and clinics.
Students in the program so far have ranged in age from 21 to 58, and many—like Loos, whose children were 3, 7 and 9 when she started—have other responsibilities outside of school. Fortunately, her family was behind her all the way. Her husband, Steven Loos '89, is an underwriter in an unusual and oddly named field called "inland marine insurance," which covers things of value—a museum exhibit or a skyscraper—only while in transit or under construction. Working out of their home, he was able to get the kids off to school when Michele had to report to her clinical rotations at 6 a.m. Today her older daughter, now 14, gives her the thumbs up on the path she has chosen: "You need to be there. You love what you do, and other people might not do such a good job as you."
Out on her clinical rotations, however, Loos faced another challenge—the open skepticism of experienced nurses who had spent two or three years preparing for the same licensure exam she and other members of the first class took after a year: "What do you mean you do the whole curriculum in a year? How can you possibly retain any of it?" Like many other direct-entry students, she responded to the skepticism by working harder, going on a trip to El Salvador to work in a hospital serving the poorest of the poor for two weeks, for example, and, upon her return, organizing equipment donations to the hospital.
Friction among nurses from different educational backgrounds isn't new, says Fetzer. There are four different paths to becoming a registered nurse: a three-year diploma, usually offered at a hospital; a two-year associate degree from a community college; the traditional four-year bachelor's degree (also offered at UNH) and the newer direct-entry master's degree. All nurses take the same national licensing exam and, with the exception of specialists such as operating room nurses, may be paid on the same scale. New Hampshire, Fetzer notes, has an unusually high proportion of nurses with two-year degrees. To help more nurses further their education, UNH enables practicing RNs to complete their bachelor's degrees at UNH Manchester, Keene State College or Plymouth State University.
UNH is also developing a statewide initiative to ease the nursing shortage by opening a bachelor's degree program at Keene State College in 2009 and an accelerated bachelor's degree program at Plymouth State University in 2010. Through collaboration with other nursing programs, the university also hopes to expand its master's and nurse-practitioner programs into the fields of nurse-midwifery, gerontology, family practice and mental health.
A woman of seemingly boundless energy, not to mention multiple degrees, Fetzer has had 32 years of experience in clinical settings while teaching in the UNH nursing department for the past 20 years. She estimates she could earn 50 percent more outside of academia. The combination of relatively low pay and the high cost of graduate school makes many nurses reluctant to become educators. Some states have instituted loan-forgiveness programs and fellowships as enticements. With their maturity, experience and commitment, the direct-entry master's graduates are not only equipped to become educators, but also excel at being leaders in clinical settings, says Fetzer, where "we really need someone who looks at systems."

Loos was already taking a systems view when, for her graduate project, she studied the need for palliative care at Wentworth Douglass Hospital. She knew that seriously ill and dying patients often suffer when medical providers and caregivers focus exclusively on the extension of life. "When a cardiologist is trained, for example," explains Wentworth Douglass chief nursing officer Sheila Woolley, "he or she is taught to save that person, to do everything to keep that heart beating. But the reality is that sometimes we can save the heart, but everything else is going. People don't want to live that way anymore." In a national study in 2000, for example, 25 percent of terminally ill cancer patients described experiencing "unbearable" shortness of breath in the last few weeks of life. Palliative care provides treatment for pain and symptoms, but it also addresses emotional and spiritual needs by helping patients identify their end-of-life goals, which might include something like "going to Hampton Beach one more time" as well as decisions on whether or not to continue efforts to cure their illness. (Loos emphasizes that palliative care also treats anyone in pain, not just the dying. But that doesn't stop co-workers from jokingly telling her she should swap her white lab coat for a black one.)
Loos and Jennifer Gagne Tenhover '91, then a nurse practitioner at the hospital and Loos's preceptor, enlisted the help of Wentworth Douglass nurses, who screened every patient admitted to the hospital in January 2006 for various symptoms and conditions. They found that roughly a third of the 335 patients might have benefitted from a palliative-care consultation.
In May 2006, Loos graduated and also presented her findings to the bioethics board at Wentworth Douglass. In December of that year, she accepted the position of palliative care coordinator at the hospital, where she works in tandem with a newly hired doctor specializing in the field. Thanks in part to Loos' prior business experience, notes Woolley, the palliative care team has been able to take the program "from infancy to a full-fledged program in a very small amount of time." In one year, Loos has reached 70 percent of the hospital's nurses on inpatient units with a series of free classes on palliative care, plus a number of hospice workers, physical therapists, administrators and others both in and out of the hospital. In February, 39 patients received palliative care consultations, a significant number for the hospital.
Loos puts up to seven miles a day on her sturdy but feminine pumps, buzzing around the carpeted corridors of the hospital. She is going, essentially, from crisis to crisis. A woman has slipped suddenly into the labored breathing signaling that she has only hours to live; an 88-year-old man is going home with the knowledge that he is in the final phases of lung cancer. A family must come to grips with the unwelcome news that their father's pain is not caused by a curable condition, but evidence that his long-symptomless cancer is now "knocking at the door." Wherever she goes, she brings an air of calm, even with a hysterical patient who has inadvertently taken a drug overdose. "It's critical to appear self-assured and competent," Loos says, "even at moments when you don't feel that way."
She and palliative care specialist Dr. Patrick Alix are sympathetic. "Try not to feel guilty if you can't take care of your dad at home," she tells the family gathered in a lounge near a large aquarium where tropical fish glide to and fro. "I'm a hospice nurse and if it were one of my family members, I would still need a whole hospice team." But they are also blunt with people who want the truth. And many do. "Am I dying?" a patient will often ask.
"There is no cure," the doctor explains to the elderly man with lung cancer, who will receive hospice care at home. "But we will make sure you have a dignified death. If you have the feeling of suffocation, morphine will be used to blunt the sensation of air hunger."
The dose of morphine required for relief in the terminally ill can be many times higher than doctors have previously prescribed. "We've had to educate pharmacy staff, nurses and doctors to insure that we can reduce suffering at the end of life," says Woolley. The palliative care program, she adds, also benefits patients' families, who are receiving much better support, not to mention the nurses. "This has been huge," she says. "It used to be incredibly sad for the nurses. They knew it wasn't right to have someone hang on in pain."
The 88-year-old man is philosophical: "So what comes, comes," he says. Gathered in the room with him are his daughter, a social worker, a chaplain, the doctor and Loos. He speaks of his 60-year marriage and how he's the last of a group of four friends who is still alive and living at home.
Some terminal patients ask to be resuscitated or treated, no matter what. "It might not be a choice I would make," notes Loos. "I've seen the results of resuscitation in that situation, and it's not pretty. But then I haven't been that 49-year-old mother dying of breast cancer."
In between visits with patients and families, Loos consults with social workers, other nurses or Alix at a nursing station. In a quiet moment, she chats with a young nurse who recently sat with her husband's grandmother in her final hours. The nurse took a break to go home and feed her baby, and when she got back, it appeared that the grandmother had awaited her return. Unable to speak, the grandmother touched thumbs with her—a gesture of affection the two had shared—before dying peacefully.
Just being with a patient, known as the "nursing presence," is an important part of palliative care, says Loos. "There are so many technological interventions and so many medications. We can do all that, but sometimes rubbing someone's back is just as important as administering [the antianxiety drug] Ativan." She recalls a patient at the hospice house. "She had the meds she needed to have, we had a plan, we had had every discussion she needed to have, but at the end of the day, she was very distressed and afraid. I was sitting next to her for 15 minutes quietly, and she said, 'Don't leave me,' and I said, 'I won't leave you.' After several minutes, she said, 'You can go now. I don't want to keep you from your work.' And I said, 'This is my work.'"
For many nurses, who must act as "a funnel" for all the technology, paperwork and documentation, "just being there" with a patient is a way of getting back to the basics, says Loos. And the relationship between nurse and patient at the end of life is an intimate one. "I almost always walk away having learned something," says Loos. "It's almost like a gift."

In the past year, one of the patients who had a profound impact on her was the late Thomas Fairchild '59, the former UNH professor of animal science, dean and interim president. Although studies show that roughly 85 percent of people would prefer to die at home, 50 percent die in a hospital, often because they have intractable symptoms that require constant monitoring. Fairchild spent his final weeks in the hospital, where he was the first to use a new palliative care room designed for that purpose. "The last week of his life, we got his pain under control," recalls Loos, "and he was able to have conversations with his kids and grandkids. He gave advice. He was teaching till the last moment."
Before he died, Fairchild told his children of his desire to write a letter to the hospital about the palliative care program. Six months after his death, two of his daughters, Karen Fairchild Reed '97, '98G and Kathryn Fairchild Francoeur '87, wrote the letter on his behalf—one of many grateful letters Woolley says that the hospital has received from families over the past year. The letter ends in this way:
"Our father said that this experience was like something from a movie or last chapter of a book. Of course, the experience of dying is surreal for everyone involved, however, he meant much more than this. He was referring to unforgettable moments of sharing love and life with his wife, children, grandchildren, friends and staff. In the 'hospice bag' given to us was a camera and journal to document these moments. Again, we are immensely grateful for having been able to capture these last times together.
"Our dad was an avid hunter; he enjoyed big game and bird hunting trips. He had hoped to run his dog in the woods before the end. However, instead of being disappointed about not making his last adventure, he said, 'I thought this trip (dying) was going to be the worst, but it has ended up being the best trip ever.' Thank you for helping our father. We are blessed to have been a part of this final journey."
Life on the Front Line
ER nurse Tim Boyd '08G talks about triage, why people go to hospitals, and why he introduces himself as 'Nurse Boyd'

Tim Boyd '08G was a photojournalist whose work appeared in the New York Times and many other newspapers before he entered the UNH direct-entry master's in nursing program at the age of 38 to start a new career as an emergency room nurse at York (Maine) Hospital.
What's it like being a male nurse?
I'm not a "male nurse," because I take care of females, too. I'm a professional. All nurses are professional. I introduce myself as "Nurse Boyd"—not "I'm Tim." I do that for two reasons. One is to go against the stereotype. The second reason is that someone who has a title is a professional. I believe physicians have earned their title as "Doctor" and I earned my title as "Nurse." The classic reaction you get from people is, "Wow, you're a smart guy. Why aren't you a doctor?" Well, I don't want to become a doctor. Would you talk to an engineer and say, "Why aren't you a lawyer?" Nursing is a profession in and of itself. I'm a nurse and I'm proud of what I do.
Why don't more men go in into nursing?
There are probably about 94 percent women in the field. I'd like to see more men in nursing, not just from a gender standpoint. I look at it as a huge pool of potential nurses. Nursing is considered a woman's job—but it's a job, it's a profession, it's a career. It's both mentally challenging and physically challenging.
Did your first career prepare you for your second?
As a journalist, asking questions comes easy to me. And I've photographed everyone from criminals to presidents, so I know a little bit about what everybody does. It helps break down the barriers for someone who might be nervous or scared. Then maybe their heart rate will decrease, maybe their blood pressure will decrease. When I'm talking to them for a couple of minutes, I'm actually assessing them: Are they having difficulty speaking? Do they have long-term and short-term memory recall? Do they know who they are, where they are, and why they are here?
Do you have any funny anecdotes?
Typically every day is funny, but a lot of it is definitely inside humor. Dark humor abounds. Not too long ago we had a sad situation where a patient had ingested a large number of pills. I was trying to get activated charcoal into the patient. We had to put a tube through the patient's nose and into the stomach, and I'm pushing this charcoal in a semi-liquid form through a small hole in the tube with a large syringe. It was extremely difficult and I'm pushing and pushing, and all of a sudden the thing slipped and this stuff went everywhere—all over the patient's face, 10 or 15 feet in the air. The nurse who's working with me is covered in charcoal, I'm covered. It looked like a giant squid had exploded. The housekeeper just happened to be walking by at that moment. You can imagine the scene.
Sounds like a scene on the TV show "Scrubs"—do you watch that?
Yeah, I do actually. Another classic show that comes to mind is "ER." There's a lot of controversy about these shows and how they depict nurses stereotypically sometimes. What I say is, so what. That's television, that's not reality, and I enjoy the shows for what they are.
What's one of the hardest things about your job?
Triage—it's tough. You have a very stoic person putting on a brave face versus somebody screaming in pain. It's hard to judge. That's why those "vital signs" tell us vital information. The person who's very stoic might be pale white, have low blood pressure, maybe has gastrointestinal bleeding—that's very dangerous. Triage is very important. It's the nurse who sees the patient first. That's why nursing is the front line in the medical field, typically.
What do you like about your job?
At York Hospital, we see 60 to 100 patients a day. There's no rhyme or reason to it. But it's also exciting, like going from 0 to 60 in a matter of seconds. We'll have a few patients and then the next thing, we've got three ambulances. I like that fast pace. And you can see almost immediately the effects of what you do.
What are your thoughts about the nursing shortage?
Nurses need to be advocates for themselves. We need to show that nursing isn't just caring, there's science, too. And with science comes professionalism and with professionalism comes respect. Pay is getting better. There are midwives, nurse practitioners, nurse anesthetists. Few people realize that nurses are researchers—they're researching things like drug-resistant staph infections. We're there with the patients, figuring out what's wrong. Not to diminish the work of physicians, but people don't go to the hospital for a physician's care. They're going because they need to be watched. It's the nurses who are there 24 hours. Nurses do so much more than people realize, and we need to recruit people.